Starting in Fall 2025, WWMG is offering new behavioral health services at select family medicine locations. This service, called the Collaborative Care Model (CoCM), is offered to support patients’ short-term mental and behavioral health needs.
Today, more than ever, many patients are in need of mental and behavioral health services. The CoCM focuses on short-term, targeted treatment for patients 10 years and older with mild to moderate behavioral and mental health conditions. Patients are referred to the CoCM program by their WWMG primary care provider.
The average treatment timeline is 4-6 months and most appointments take place at the clinic where your primary care provider is located. Patients who need a higher level of care will be referred to WWMG Psychology or other behavioral health providers in the community.
This service is currently offered at Marysville Family Medicine and Whitehorse Family Medicine.
Who needs Collaborative Care?
Patients most often referred to CoCM are those who are feeling anxious or depressed, experiencing grief or loss, or going through a life transition.
But there are other possible reasons for referrals to CoCM. For example, if you would like help reducing or quitting smoking, improving sleep, or support for managing your medications, these are all goals that our Behavioral Health Care Manager (BHCM) can help you to achieve.
WWMG primary care providers can refer eligible patients to the CoCM program.
What is an appointment like?
The first CoCM appointment will be in person at one of our family medicine clinics, and usually lasts around 60 minutes. At this visit, the BHCM will gather information and get to know you. Your Care Manager will speak with you about your goals and how to help you achieve them. After that, follow-up visits are generally 20-30 minutes as you work towards your treatment goals.
Visits can be accomplished face-to-face, through virtual appointments, or as a brief phone call to check in. Patients in CoCM are usually seen every other week for 4-6 months—this will be based on your specific needs and goals. As you improve and make progress toward your goals, you may need less frequent visits.
Who is on the patient’s care team?
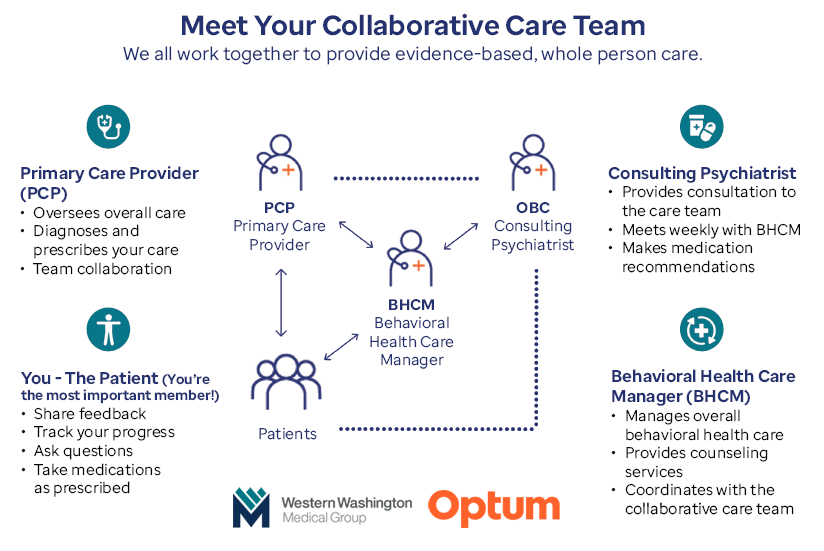
Our clinics aim to provide holistic care to our patients, focusing on each person’s physical as well as mental health. To do so, we’ve brought a team of providers together in the CoCM with one goal in mind: to help you, the patient, meet your treatment goals.
In this model, your primary care provider works with the BHCM and a consulting psychiatrist to design and implement your treatment plan.
All members of the collaborative care team will have access to case notes in WWMG’s electronic medical record system and will communicate regularly about your plan of treatment. This will help to ensure whole-person care.
Is CoCM the same as regular counseling/therapy?
Collaborative Care is different than traditional therapy because it is short term and, in general, the visits take less time. If you’re finding that you want or need longer-term treatment, your CoCM team can discuss a referral to traditional or specialty behavioral health services.
What does it cost?
A patient’s copay or deductible for this model is typically lower than the copay or deducible for traditional behavioral health services, because it is billed as a Primary Care visit.
In the Collaborative Care Model, the copay or deductible is only charged once a month, even if you meet with the BHCM multiple times during a month.
As with any service, out of pocket costs will vary depending on the service provided and your insurance coverage benefits. Contact your insurance provider to find out your coverage level and what the expected cost-share percentage or copay would be. CoCM billing codes: 99492, 99493, 99494
If you’re interested in this program, talk to your WWMG primary care provider about a referral to CoCM.
 WWMG’s Collaborative Care Model is provided in partnership with Optum Behavioral Care.
WWMG’s Collaborative Care Model is provided in partnership with Optum Behavioral Care.
(click on image above to enlarge)